My brother Roger is recovering remarkably well. He will come home from the hospital tomorrow. He was quickly getting out of bed on his own and walking with a walker. And as of this morning, 3 days post-surgery, he is only taking Tylenol for pain (what?!?). He comes home tomorrow. He has a long road ahead of him, 8 weeks immobilized and then he starts 5 day a week physical therapy to reteach his reconstructed and a bit less muscular leg to balance and walk. Thank you everyone for your love, prayers and support.
As it turns out, on the day my brother received his date for surgery I also received mine. On November 19th I had my MRI on my meningioma. It had been two years, in 2016 my annual MRI showed no progression so it was safe to wait two years this time. I received the MRI results in my patient portal account (MyChart). And it wasn’t anything dramatic, per se:
Subfrontal meningioma with extension into the bilateral olfactory groove regions currently measures 33 x 31 mm which is slightly enlarged from prior exams including 32 x 28 mm on 8/15/2016 and 27 x 26 mm on 4/28/2014. Coronal diameter of 25 mm is unchanged from 8/15/2016 and slightly increased from 21 mm on 4/28/2014. Mild focal edema signal adjacent to the posterior superior right aspect of the mass is unchanged from 8/13/2015 although with progression since 4/28/2014. Slight edema signal at the left superior lateral aspect represents slight progression.
But even to the untrained eye (I have lots of experience but zero training), I was pretty sure my neurosurgeon was going to want to take it out this time. It hadn’t grown a lot, but it had grown, and as I like to say, “It isn’t ‘not growing’.” And as you can see it is not small, it is golf ball size.
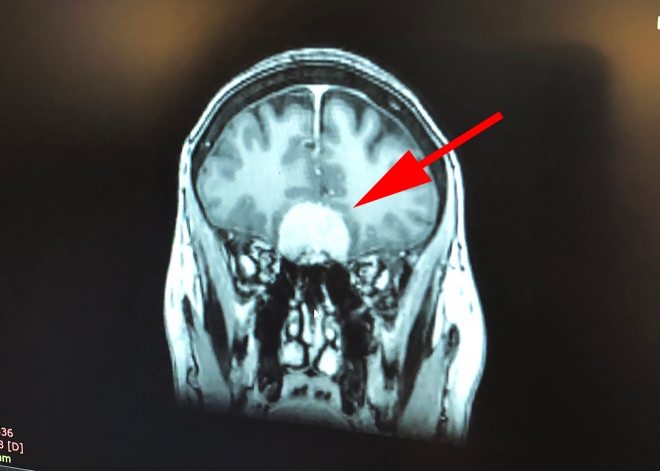
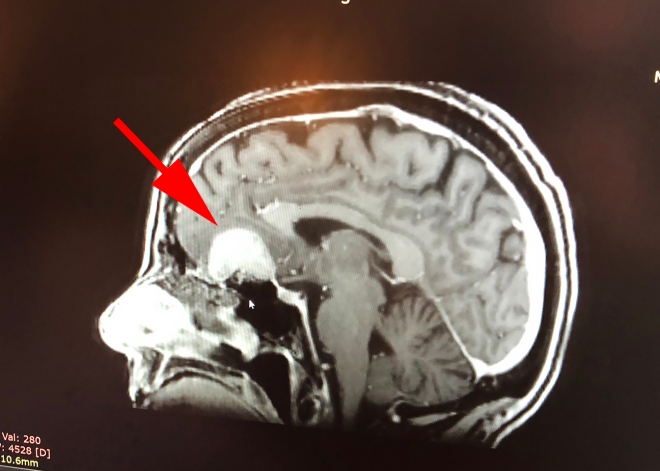 By the time I went to my appointment with Dr. Michael Sisti at Columbia Presbyterian on December 6th I was so prepared for the news that I literally didn’t bat an eye. I did ask him if I could take a photo of his screen with my MRI on it. I told him how I always tell my friends, “You can’t miss the tumor, you can see it from across the room.” He said, “If your friends can’t see this tumor, you need new friends!” So my friends – there it is.
By the time I went to my appointment with Dr. Michael Sisti at Columbia Presbyterian on December 6th I was so prepared for the news that I literally didn’t bat an eye. I did ask him if I could take a photo of his screen with my MRI on it. I told him how I always tell my friends, “You can’t miss the tumor, you can see it from across the room.” He said, “If your friends can’t see this tumor, you need new friends!” So my friends – there it is.
I had a few questions in regard to scheduling the surgery:
- How long do I need to be out of work? About one month.
- How long will I be “disfigured”? Not long, worst case scenario a really bad black eye on one side.
We had a trip to Florida planned for January 25th, visiting family and friends, coming home on Super Bowl Sunday. He operates on Tuesdays and Wednesdays, so Tuesday, February 5th it is.
I just re-listened to the recording I took of my appointment with Dr. Sisti (which as it turns out was the only time I will see him prior to my surgery). Here are some of the details:
- Type 1 meningioma
- My tumor is taking the well-known super slow growing, benign, natural history of this disease
- In a neurologically non-critical location
- Pressing on one of my two olfactory nerves
- A year or two away from pressing on my optic nerve
- It is too large for non-surgical treatments
He described the surgery as “nothing you’d ever really want to have”. His preference is to come in from the right side, the non-communication hemisphere. He makes an incision behind my hairline, where a plastic surgeon would make the incision for a facelift (no, I can not throw a facelift in, I asked!). And no, he does not shave my head (so there’s that!). He then “reflects the scalp down” – this is a very gentle way of saying he is going to peel my forehead down (yummy).
Then they use a computer, to make a minimum access opening that looks like a half-moon above my eye. He joked “Although there’s nothing really minimal when it’s your skull and someone is opening it!” No, indeed. They glue the bone back in with bone cement when they are done and he said I won’t even be able to feel a bump or line once it has healed.
He will be doing a surgical resection of the tumor. Although if he has a choice between “normal life or normal scan” he will choose normal life, which in this case means saving my sense of smell. If he had to he might leave a small portion in rather than nicking my olfactory nerve. It is “not a particularly painful surgery”, side effects include soreness, headache, a feeling of disconnection, and a feeling that someone “beat the hell out of you”.
After surgery I will be on an anti-convulsive medication and steroids. The steroids are necessary because my brain will literally fill the void left from the removal of the tumor, which is a shock to the brain. And for what ever reason, the thought of my brain moving in to fill that space makes me really nauseous!
I will spend the first night in the Neuro ICU and then be moved to a semi-private room for likely 2 more nights, but they don’t rush you out, you need to be functioning independently.
They will know the morning after the surgery if I have maintained my sense of smell, “Smell a cup of coffee? We’re good. Can’t smell a cup of coffee, we’re not so good.”
They will do five years of monitoring (MRI scans) to check for local recurrence or new meningiomas (he does not expect new ones, since I have had just the one for what he imagines is well over a decade). If surveillance picked up a new one it would be treated non-surgically. So just this one surgery, thats the plan!
Things to remember: it’s not like it’s brain surgery – although they open your skull and they worry about effects on your brain – they are not operating on your brain. And secondly, I’m not just losing a tumor, I’m expanding my mind (brain)!
And here we go!
Did I mention, it’s always something? 🙂